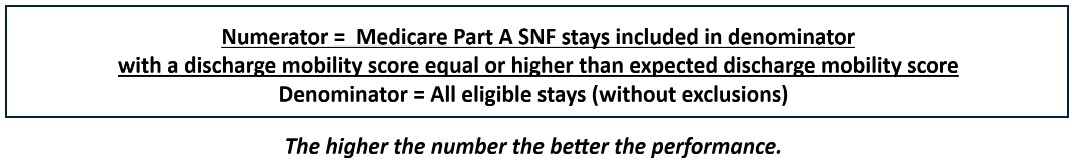
The Quality Measure for Discharge Mobility Score estimates the percentage of short-stay residents who meet or exceed their expected discharge mobility score. This is an Outcome Based Measure and is part of the Quality Reporting Program (QRP). It further impacts Care Compare and Five Star.
The Mobility items and coding utilized for this measure are:
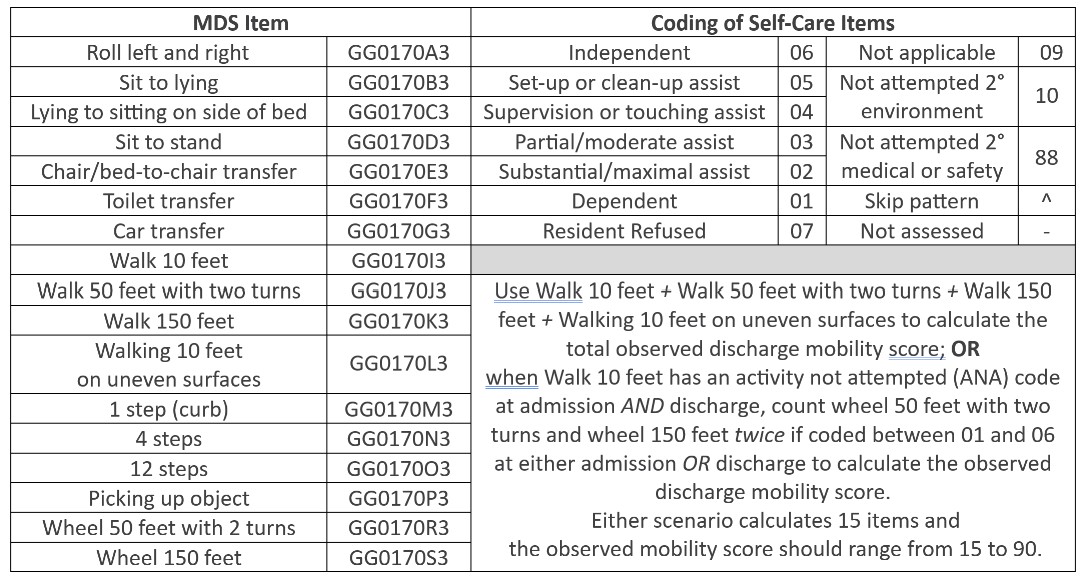
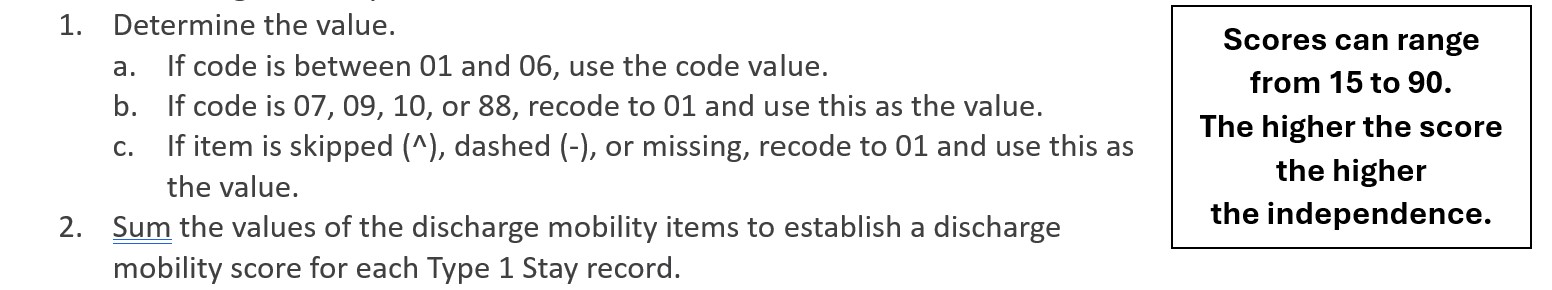
The numerator is the total number of SNF Medicare Part A stays, or Type 1 stays, in the denominator, with an observed discharge mobility score equal or higher than the calculated expected discharge mobility score. The observed discharge mobility score is calculated as follows:
The expected mobility discharge score is calculated using an intercept and regression coefficient calculation, which factors in the covariates.
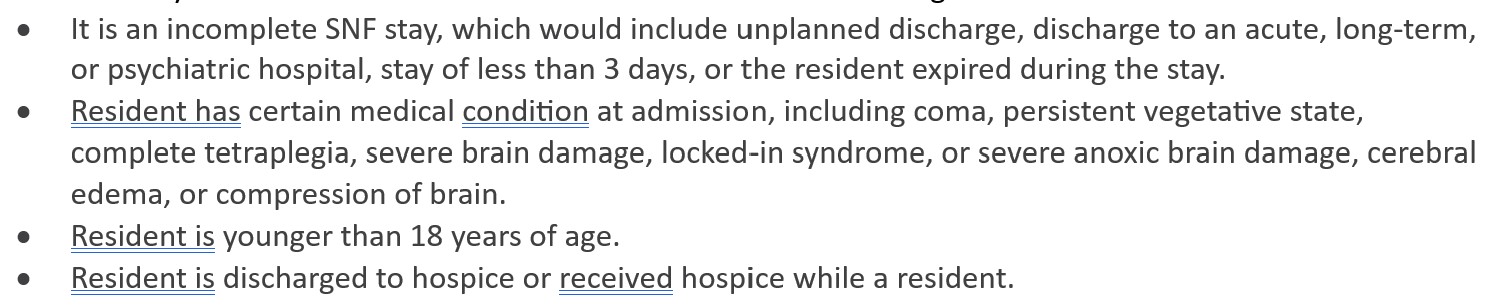
The denominator for this measure is the total number of Type 1 SNF Stays, except those meeting the exclusion criteria. SNF stays are excluded from this measure based on the following:
The target period for this measure is 12months. All stays the resident had in the 12 months are included.
This measure is risk-adjusted. The covariates for risk-adjustment are as follows:
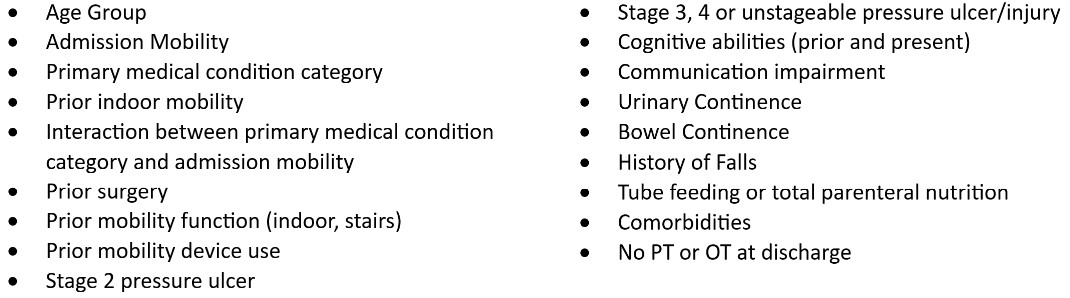
Data for these covariates is taken from the admission assessment included in the targeted SNF stay.
This Outcome Based Measure affects the QRP, as stated above, and as such impacts the Annual Percentage Update (APU). The APU can lead to an up to 2% reduction in payment if data is not submitted for 100% of MDS assessments or performance is poor.
To ensure successful outcomes, an Interdisciplinary Team approach should be utilized to address issues and progress the resident toward a more independent level of functional mobility:
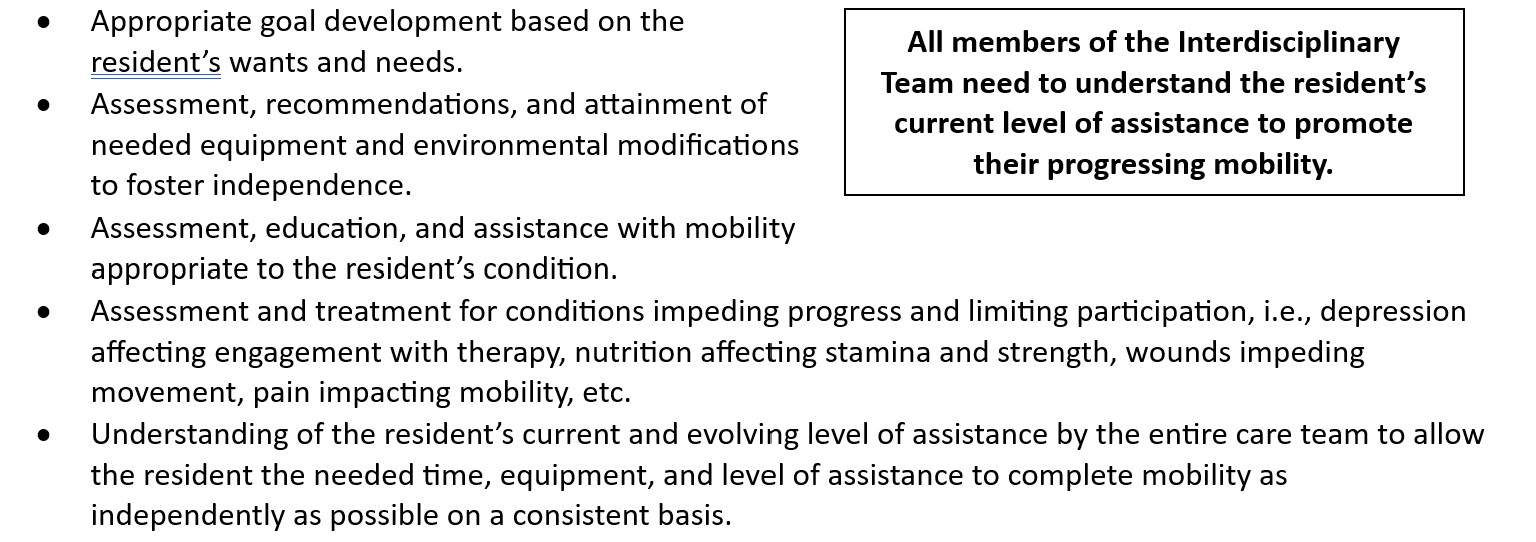
To foster positive outcomes, teamwork among the Interdisciplinary Team, the resident, and their family is essential to progress.
To learn more about the Quality Reporting Program, go to https://www.cms.gov/medicare/quality/snf-quality-reporting-program.