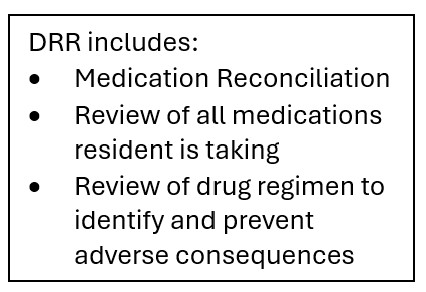
The Drug Regimen Review (DRR) conducted with follow-up for identified issues quality measure identifies the percentage of Medicare Part A SNF stays where a DRR was performed at the time of admission and timely follow-up with the physician occurred each instance where a potentially clinically significant medication issue was identified during the stay. This measure impacts Care Compare.

The numerator for this measure is the number of Type 1 Medicare Part A SNF stays, who meet both of the following:
1. A DRR was conducted on admission, resulting in one of the following:
- No potential or actual clinically significant medication issues were found (N2001= 0); OR
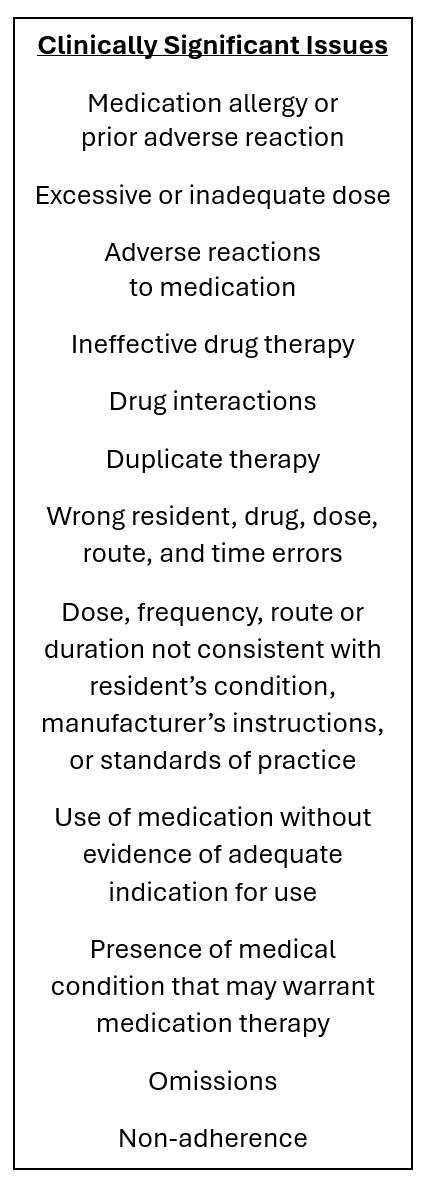
- Potential or actual clinically significant medication issues were found (N2001 = 1) and then a physician or physician designee was contacted and prescribed/ recommended actions which were completed by midnight of the next calendar day (N2003= 1); OR
- Resident not taking any medication (N2001 = 9); AND
2. Follow-up occurred each time a potential or actual clinically significant medication issue was identified during the stay (N2005 = 1); OR no potential or actual clinically significant medication issues were identified since admission; OR resident not taking any medications (N2005 = 9).
The denominator is the total number of Type 1 Medicare Part A SNF stays during the reporting period
If a resident has multiple stays during the target 12 months, all stays are included in the measure.

Exclusions for this measure include Type 2 SNF stays - Resident died during SNF Stay and there is a PPS 5-day Assessment (A0310B = 01) and a matched Death in Facility Tracking Record (A0310F = 12). There are no covariates for this measure.
For this measure, the higher the score the better the performance. A national average observed score is calculated for this measure. The current score is 95.1 for the period of 10/1/2023 through 9/20/2024.
This measure can be addressed in multiple ways by the Interdisciplinary Team and should be, particularly if your facility percentile is below the national average observed score.
The medical record should be a resource for DRR through review of hospital records, most recent history and physical, transfer documents, discharge summaries, medication lists/records, and clinical progress notes. Conversations with the transferring facility, other clinicians, the resident, and their family can be useful for clarifying the medical record.
Utilize QAPI to address facility and resident level opportunities for improvement. QAPI opportunities at the resident level include meeting monthly with the pharmacist to review the individual’s medication list.
Involve the medical director in reviewing resident records and medications. During pre-admission and admission, carefully review the resident's medication and regimen and determine if there are any possible issues.
Utilize the State Surveyors’ Medication Regimen Review, Medication Administration, and Unnecessary Medications, Critical Element Pathway to assist in establishing processes and procedures.
The overall goal for improvement with this quality measure is to limit adverse events due to medications.
To learn more, go to Skilled Nursing Facility (SNF) Quality Reporting Program (QRP) | CMS.