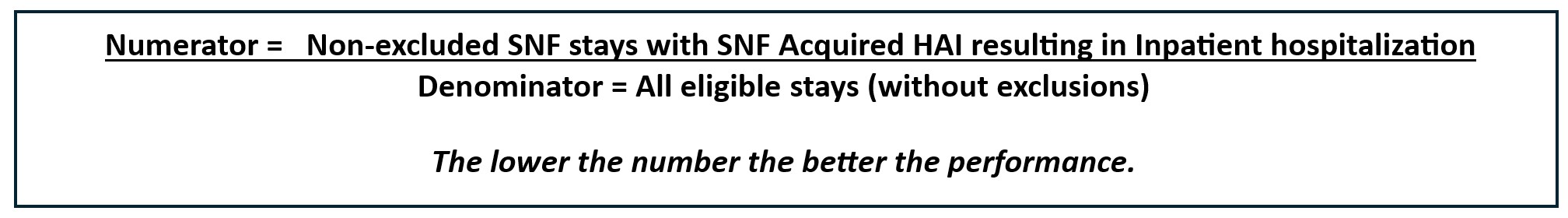
The Quality Measure for SNF Healthcare-Associated Infections (HAI) Requiring Hospitalization evaluates the risk standardized rate of Healthcare-Associated Infections acquired in the SNF resulting in hospitalization. This Claims Based Measure is part of the Quality Reporting Program (QRP). It further impacts Care Compare.

Eligible SNF Medicare Part A stays for the collection period are identified by reviewing final Medicare Part A Fee for Service claims and matching beneficiary and facility identifying data. The collection period for this measure is a Calendar Year (CY).
SNF stays are excluded from the measure if the following is true:
· Resident was under 18 years of age at start of stay
· Length of stay in SNF was less than 4 days
· Resident was NOT continuously enrolled in Medicare Part A during the SNF stay,365 days prior to the measure period, and 3 days after the end of the SNF stay
· Resident was NOT discharged from an acute facility within 30 days prior to SNF admission
· Resident discharged from SNF to federal hospital
· Care received outside the 50 states, District of Columbia or Puerto Rico, and U.S. Territories
· Medicare did not pay for the SNF stay
· Data missing on variables used in measure construction or risk adjustment
· Stay occurred in a Critical Access Hospital (CAH) swing bed
CMS does provide a list of ICD-10 codes for HAIs on the SNF QRP webpage under downloads within the SNF QRP Claims Based Measure Supplemental Files. There are close to 800 ICD-10 codes listed.
The measure calculation accounts for an incubation window. This window begins on or after the fourth day of the SNF stay and within 3 days of SNF discharge. If a measure is marked as present on admission (POA) on the Inpatient (IP) Hospital claim and the ICD-10 code is on the SNF QRP Claims Based Measure Supplemental Codes workbook, it is included in the numerator. There is also a 14-day repeat infection timeframe (RIT) to exclude preexisting infections.
· If the number of days between IP stays is <14 days, search for HAI related conditions in prior IP stay
- If one is found, exclude stay
- If one is not found, include stay
· If the number of days between IP stays is >14 days, include stay

This measure is risk-adjusted. The covariates for risk-adjustment are as follows:
· Age and sex categories
· Original reason for Medicare entitlement
· Surgical procedure categories from prior proximal acute care stay
· Dialysis, without ESRD, during prior proximal acute care stay
· Principal diagnosis of prior proximal acute care stay
· Length of prior proximal acute care stay
· Number of IP stays in prior 365 days prior to SNF admission – excludes IP stay prior to admission
· Utilization of intensive care unit (ICU) or cardiac care unit (CCU) during prior proximal acute care stay
For this measure, a National Observed Rate is determined as well as a Provider-level final score. This Claims Based Measure affects the QRP, as stated above, and as such impacts the Annual Percentage Update (APU). The APU can lead to an up to 2% reduction with poor performance.
An Interdisciplinary Team approach should be utilized to address issues related to infection prevention including:
· Perform infection control assessments and identify areas to be addressed
· Make infection prevention a critical element of a Quality Improvement Plan utilizing data analysis and evidence-based prevention strategies
· Train and educate staff, volunteers, residents, and families about infection prevention, including handwashing, PPE use, and various infection prevention precautions
· Complete staff competencies on a regular basis, including planned and unplanned checks, for continued educational purposes
· Develop outbreak management and response planning
· Use data analysis of infection rates and outbreaks to develop infection surveillance systems
· Offer updates to staff, residents, and families regarding infection prevention policies and safety measure
· Involve leadership in communication of infection prevention
There are numerous resources available related to infection prevention and control:
· NACCHO
· Infection Control for Healthcare Providers | Infection Control | CDC
· Infection Prevention and Control Resource Center | Joint Commission
To learn more about the Quality Reporting Program, go to Skilled Nursing Facility (SNF) Quality Reporting Program (QRP) | CMS.